Gut Dysfunction From Hell Yet Unremarkable Medical Findings: Part I
/So Much Dysfunction, So Little Answers!
As functional health practitioners we speak with clients on a regular basis about their health and life histories. Within the narratives, long histories of gut distress seem to be a commonality. Clients from all walks of life tell the tales of how they recall mild to moderate gut issues such as bloating, stomach aches, constipation, diarrhea, and poor digestion from a very early age. They go on to explain how their parents may have taken them to their primary care physician for routine medical workups yet no real answers were uncovered.
With no answers one often falls into the trap of thinking "this is just how my body is and I need to learn to live with it". Others may experiment with trying to make correlations on their own and avoiding lifestyle factors and foods that they know to be symptom triggers.
Through this process, one's symptoms may resolve to a point where the urgency to identify root causes is no longer there. In other words, life goes on for people and without major life altering symptoms there is little motivation for further investigation. This often does not mean, however, that root causes have been addressed solely because symptoms have been mitigated. Quite the opposite often occurs.
You see, symptoms and chronic health complaints are indeed common nowadays but they are not normal. Symptoms are our body’s alarm system, signaling that there are imbalances that need to be addressed. Just as turning off a fire alarm in a building without finding and extinguishing all the fires will lead to an inferno, suppressing symptoms in the body without identifying and addressing the root causes will lead to metabolic chaos® and ultimately dis-ease.
The lack of addressing true root causes often allows dysfunction to proliferate insidiously beneath the surface. The child that was once experiencing mild to moderate gut issues is now an adult suffering with a wide range of chronic health challenges such as fatigue, poor libido, unstable moods, pain, lowered immunity, autoimmunity, and the list goes on. Or, it could be a specific diagnosis such as Fibromyalgia, Chronic Fatigue Syndrome, or something more foreboding as in waking up one day to a cancer diagnosis.
With years of hidden dysfunction, it is easy for life events such as job stress, death of loved ones, mold exposure, head injuries, major acute illness, divorce, etc. to be the catalyst that lights the match and allows the inferno of chronic illness to roar. Making correlations between past histories of mild to moderate health challenges and major life events is what is necessary to identify true root causes. This gives one an explanation of how health conditions that seemingly come out of the blue are actually the result of dysfunction that has been brewing for many years.
The Status Quo of Gut Dysfunction and More!
If the above paragraphs describe you please know that you are not alone. We fully relate to this trajectory of experiences and all the frustration, loss, and fear that ensues. We both have had our share of booking consults with many gastroenterologists and other specialists in hopes of identifying the cause of our woes only to be disappointed by unremarkable findings and an RX for a drug to hopefully help manage the symptoms.
Within the world of Conventional Medicine, the standards for investigating gut dysfunction most often begin with routine blood labs, upper endoscopies, and colonoscopies. These measures are important and wise to take to rule in or out serious medical diagnoses such as obstructions, inflammatory bowel disease, cancer, and more.
The frustration comes in, however, when these invasive investigations do not provide answers or action steps beyond trialing various meds in hopes they will help provide relief. And, even if one of the before-mentioned investigations did reveal a medical diagnosis, they do not provide clarification of true root causes. Furthermore, obtaining one of these diagnoses most often results in managing symptoms with drugs versus addressing root causes, balancing the matrix and inner terrain, and helping the body to return to homeostasis.
What Are The Root Causes of Gut Dysfunction?
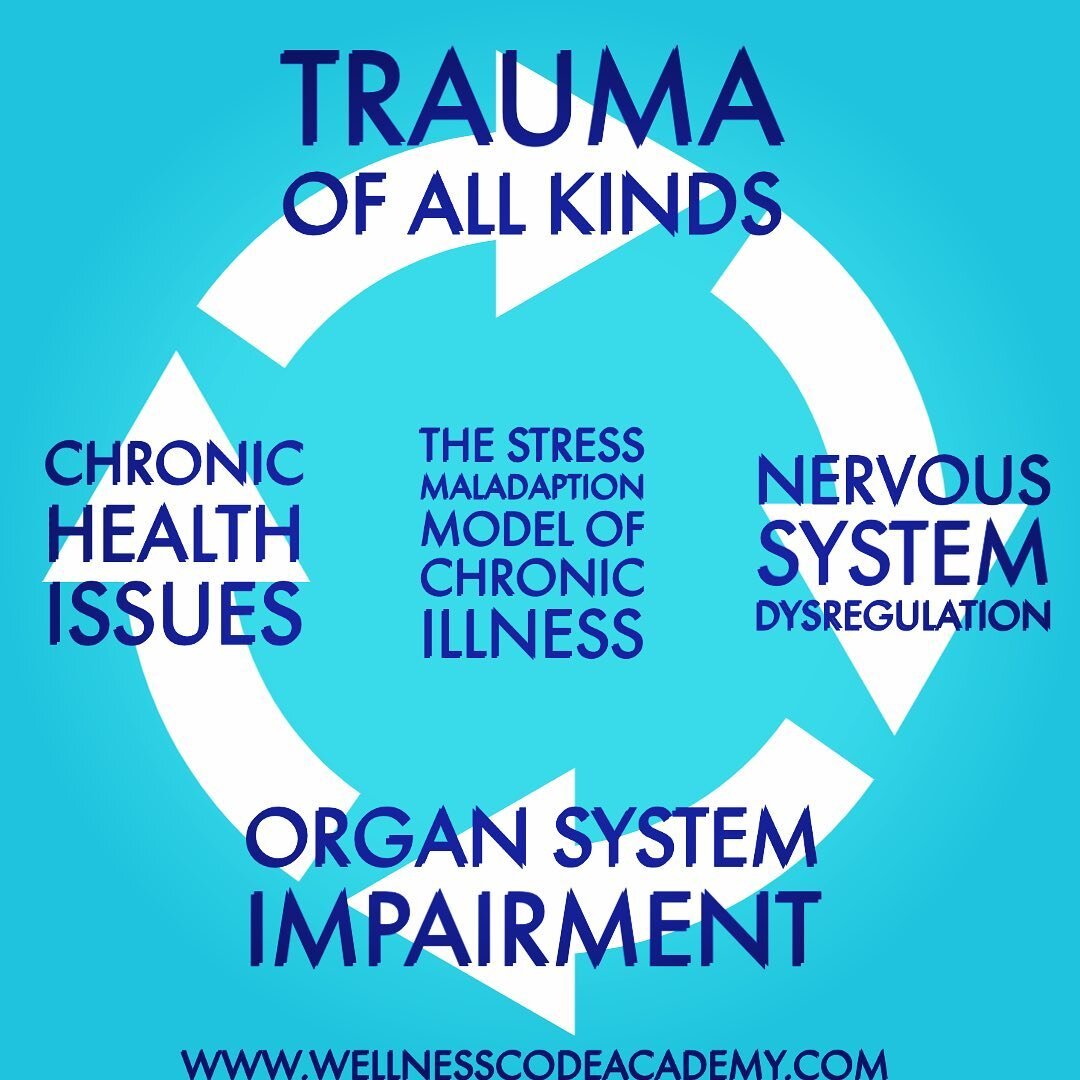
In both our personal and professional experiences, we see the root causes presenting in a hierarchy with the first rung of the ladder being a perpetually engaged stress response and the last being metabolic choas© - with several factors in between. Also please know that we will not be listing every single cause but rather giving an overview of the main ones.
Perpetually Engaged Stress Response
The stress response, also known as fight or flight, is meant to be a short-term, life-preserving mechanism ONLY. It is meant to activate when we need it most, such as maneuvering our car to avoid a deadly collision, fighting off an attacker, or even pushing hard in the last mile to win that marathon. After this it should subside so our bodies can return to a state of rest and digest. When this mechanism is chronically activated by non-emergency situations such as a toxic relationship, a soul-sucking job, or a painful memory that we keep reliving in our mind's eye, the body’s main stress hormones (cortisol and adrenaline) are continually bathing our organs, cells, and tissues. Overtime, these hormones will break the body down and cause issues such as lowered immunity, muscle tension, headaches, chronic inflammation, impaired cognitive function, anxiety/depression and much more! Typically, the first bodily system to be adversely affected by a chronic stress response happens to the be the digestive system.
Low / High Stomach Acid
With the digestive system being the first organ system that takes the brunt of stress, natural stomach acid production slows ways down or possibly even comes to a halt. This is because when the body is preparing for an emergency, it is not concerned about digesting one's last meal. Low stomach acid often presents as symptoms of acid reflux/GERD, These symptom often spur people to visit their doctor and be handed a script for acid reducers or proton pump inhibitors such as the infamous purple pill, Nexium.
While we observe low stomach acid to be a common trend, it is important to realize that too much stomach acid can also happen. Just as too little stomach acid can cause a disruption in gut motility so can too much. Additionally, hyperacid production can also lead to gastritis and put one at risk for ulcers and other erosive conditions. Three common causes of high stomach acid are diet, a perpetually engaged stress response, or an acute trauma such as surgery or an accident.
Seeing that supplementing with hydrochloric acid supplements (which is a common practice) could cause further issues in one does not truly have low stomach acid, it it always wise to test stomach acid levels. There used to be a test that was once readily used by GI docs called the Heidelberg Test that could accurately assess HCL levels. Unfortunately now there are only handfuls of doctors using it and it can be difficult to find access to it. But, you may be one of the lucky ones and have a doctor in your area that uses it.
Dysbiosis and Chronic GI Infections
Our stomachs are meant to be highly acidic in order to kill opportunistic, pathogenic microbes that hitch a ride on food, water, and air. Without optimal levels of stomach acid, it is only a matter of time before microbial overgrowths or pathogens take a foot hold and become a source of hidden stressors on the body. Microbial overgrowths refer to when a bacteria, yeast, or fungus that is a normal part of the human microbiome are no longer kept in check and balance. Pathogenic infestations on the other hand involve the presence of microbes that are not ever part of the normal human microbiome. Examples of such organisms would be parasites such as giardia or cryptosporidium parvum, bacteria such as salmonella or campylobacter, yeasts/fungus such as microsporidia, and viruses such as norovirus or rotavirus.
Leaky Gut
With low stomach acid production, microbial overgrowths, and pathogenic infestations, the epithelial lining of our digestive tract becomes inflamed. This lining is our first layer of defense against the outside world in which we interact with via ingestion and respiration. The inflammation then causes the lining of the gut to become overly permeable and allow undigested food particles, microbial metabolites, and possibly microbes themselves to leach into the blood stream. This in turn triggers the immune system to mount a response which then cascades into a widespread inflammatory response to a molecule that should have remained and been properly assimilated within the digestive tract. Widespread inflammation can manifest is a various ways such as fatigue, headaches, acne, hives, depression, and much more.
Food Intolerances
When the gut goes awry, pathogenic microbes have taken hold, and the lining becomes leaky, it is common for the immune system to begin hyper reacting to a variety of foods we were once able to eat with no issues. This can include even the healthiest of foods. To be clear, food intolerances are not a root cause but rather a symptom of everything already mentioned.
Celiac Disease / Non-Celiac Gluten Intolerance
Two other points that we need to mention at this juncture are gluten intolerance and Celiac Disease. While Celiac Disease is a genetically based, autoimmune issue and gluten intolerance is not, the two can be equally as damaging. For the longest time we embraced the research that supports the inflammatory effects of gluten and we made a point to avoid gluten however, we failed to be strictly gluten free.
We thought, “How much could a little bit hurt us, especially if we eat sprouted and organic sources of it or only consume "very small amounts" as can be found in some organic salad dressing from time to time?”.
Oh boy, were we wrong! We failed to understand (or shall we say accept and embrace) that even a small amount of gluten (as little as one crouton) is capable of creating lasting inflammation for up to 6 months; especially in a body where metabolic chaos® is well under way. And then, through a series of labs, scans, and an intestinal biopsy during the time leading up to a SIBO discovery, Jennifer found out she had Celiac Disease. This had caused significant damage in the form of villous atrophy throughout the midsection (the jejunum) of the small intestines - where the majority of digestion, absorption, and assimilation occurs.
SIBO (Small Intestinal Bacterial Overgrowth)
SIBO, or small intestinal bacterial overgrowth, is just that—an overgrowth of bacteria in the small intestine, the part of your digestive tract where the nutrients from food are absorbed for your cells to use as fuel. The small intestine should be relatively sterile in relation to the large intestines. SIBO is a condition of dysfunctional motility and then gut microbes that belong in the large intestine and colon become translocated into the small intestine.
Symptoms of SIBO can include bloating, especially after meals, gas, indigestion, gastrointestinal reflux, constipation or diarrhea, abdominal cramping or pain, nausea, vomiting, anxiety or depression, widespread pain, fatigue, and more.
Most conventional doctors don’t recognize SIBO as a real condition and instead, they diagnose patients with “IBS” and send them off with a prescription for anti-nausea aids, proton-pump inhibitors, and/or antibiotics—the worst offenders when it comes to gut health—or laxatives. Even among the doctors who do acknowledge that it exists—usually functional medicine doctors—they often don’t explain to their patients that SIBO at its core is a product of system-wide imbalance and a fractured brain-gut connection that has persisted for many years, and ultimately has impaired gastrointestinal motility.
To read an in-depth reference study about how PPI's (Proton Pump Inhibitors) are a large contributor to SIBO, click HERE.
Widespread Metabolic Chaos©
When all that has been previously discussed goes on without resolve, the end result is widespread dysfunction, down regulation of cellular energy, and suboptimal organ function. Within this state many epigenetic changes occur in the body. The genes of health turn off and the genes of illness turn on. Overtime symptoms morph into illness and eventutally dis-ease states.
Unraveling Gut Dysfunction!
Stay tuned for part II where we will be providing a description of a comprehensive, functional investigation into gut dysfunction and how we go about unraveling it and other corresponding health challenges.